
6.1 million lives covered by Delta Dental of Michigan
Thank you for your continued dedication to our members!
For the record
How do Michiganians stack up against the nation when it comes to dental benefits? Consider these facts from the National Association of Dental Plans.
- An estimated 86 percent of the Michigan population has dental benefits, compared to 80 percent of the national population.
- Of those with dental benefits nationwide, 89.6 percent receive benefits through a large group plan.
- The number of adults nationwide who had a dental check-up in the last 12 months included:
- 61 percent with dental benefits
- 37 percent without dental benefits
Source: The National Association of Dental Plans, “Michigan: Dental Benefits Fact Sheet,” web.
Back to top
Customer service and operations corner
There are a few things you can do to help speed up your claim submission timeline. Here are a few tips:
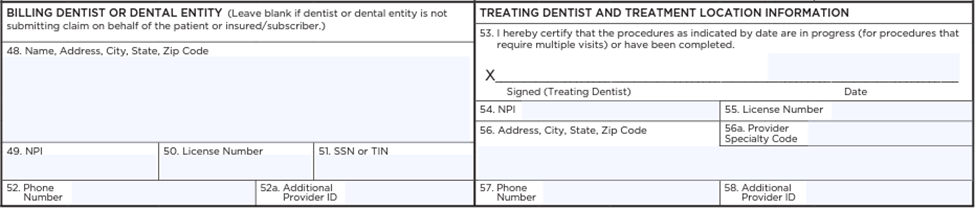
- The most preferred claim form is the ADA standard dental claim form.
- The “Billing Dentist” and “Treating Dentist” fields are some of the most important fields to be completed.
- When submitting a claim, ensure you’ve completely filled out the “Billing Dentist or Dental Entity” boxes (48–52) and the “Treating Dentist and Treatment Location Information” boxes (53–57).
Back to top
Crown coverage with Healthy Michigan Plan
Michigan adults with Medicaid now have expanded benefits thanks to the Michigan Department of Health and Human Services’ Medicaid redesign. Included in the benefit changes that took effect April 1 are indirect restorations (crowns).
If you treat Healthy Michigan Plan members, note the crown coverage policies:
- Crowns are covered once every five years.
- Coverage is limited to full metal crowns on the first and second permanent molars.
- Porcelain and porcelain fused to metal crowns are limited to permanent first and second premolars, canines and incisors (4–13, 20–29).
If you elect to do a more costly crown on the first and second permanent molars, benefits will be paid at the resin crown fee.
As always, it’s important to verify benefits before rendering services. If your office staff is scheduling an appointment and the patient says they have Medicaid or Healthy Michigan Plan:
- Confirm they are covered by Health Alliance Plan (HAP), McLaren, Priority Health or Upper Peninsula Health Plan (UPHP).
If they are unsure, ask if they have their Delta Dental ID card, or you can use the Dental Office Toolkit to search for the patient.
Back to top
New options added to CE
course lineup

The list of CE courses Delta Dental provides at no cost for participating providers and their staff is growing!
Ethics and Jurisprudence was added in July, and covers dental ethics, professional definitions (RDA, RDH, dental therapist, dentist, specialist), delegation, supervision, assignment, dental record requirements and jurisprudence.
- Course participants will learn the rules regarding assignment of duties to various dental professionals and staff, the standards of record keeping according to the ADA and various aspects of jurisprudence.
- One CE credit can be earned by completing this course.
- This program fulfills the State of Michigan requirement for ethics and jurisprudence.
Infection Control was added earlier this year and reviews CDC guidelines on infection control in the dental office.
- Course participants will review CDC guidelines on infection control in the dental office, while also reviewing hand hygiene, PPE, respiratory hygiene, sharps safety, injection safety, sterilization, environmental safety, waterline safety and program development.
- One CE credit can be earned by completing this course.
- This program fulfills the State of Michigan requirements for infection control CE.
Visit www.deltadentalmi.com/onlineeducation for a full course list and more details.
Delta Dental Plan of Michigan Inc. is an ADA CERP-recognized provider.
Back to top
Updated manuals in DOT
You can now access updated provider manuals for Delta Dental Healthy Kids Dental, Healthy Michigan Plan (including Medicaid and MI Health Link) and/or Medicare Advantage in the Dental Office Toolkit®.
The newest versions account for changes that went into effect April 1 as part of the Michigan Medicaid redesign from the Michigan Department of Health and Human Services. As you continue to serve Delta Dental members, please keep in mind:
- Benefits should be verified before the time of service.
- If a Delta Dental Medicare Advantage or Medicaid member requires services not covered in their benefit plan, be sure to obtain a signed private pay form from that member before rendering services. Include the form as part of the patient record. You may use any form for the private pay agreement as long as it includes the fees associated with the non-covered service, the responsible party’s signature and the date. (See Delta Dental’s sample form here). Participating dentists should reference their Delta Dental agreement about any charges for non-covered services provided to Medicare Advantage members or those with Medicaid benefits.
Back to top
Timeliness standards of care
As part of our Delta Dental Healthy Kids Dental, Healthy Michigan Plan and/or TriState Advantage network(s), you have a critical role in our members’ oral and overall health.
If you are scheduling patients who have Healthy Kids Dental, Medicaid, Healthy Michigan Plan or MI Health Link benefits, remember that they must be seen within a specific time frame. These benchmarks are required by the Michigan Department of Health and Human Services. The benchmarks are included in your participation contract or below for general practitioners or pediatric dentists:
- Urgent care—see within 48 hours
- Routine services—schedule within 21 business days
- Preventive services—schedule within six weeks
- Initial appointment—schedule within eight weeks
- Emergency services—provider must be available immediately, 24/7
If you are unable to meet these standards, please contact your professional relations representative.
Back to top
Removing barriers to care
The leading unmet health care need for millions of U.S. children and adults with a disability is adequate dental care. Delta Dental’s Special Health Care Needs Benefit reduces barriers to care by providing eligible members with enhanced benefits.
If you have a member with this benefit as part of their plan, they may receive:
- Additional visits to the dentist’s office and/or consultations that can be helpful prior to the first treatment to help them learn what to expect and what is needed for a successful dental appointment. Additional exam benefits will be allowed for this purpose.
- Up to four total dental cleanings in a benefit year.
- Treatment delivery modifications, including anesthesia and nitrous oxide, necessary for dental staff to provide oral health care for those with sensory sensitivities, behavioral challenges, severe anxiety or other barriers to treatment.
Before rendering services, check the member’s procedure eligibility in the Dental Office Toolkit® (DOT). If the member’s record has been updated to allow for additional services under this benefit, there will be a message in DOT confirming this.
- If there is not already a message but the member says their Delta Dental plan includes the Special Health Care Needs Benefit and they have a qualifying special health care need, you should include code D9997 on the initial claim submission for the patient.
- After this first claim processes, the member’s procedure eligibility will update accordingly.
Note: There is no age limit on these benefits. When looking in DOT, the “Special Health Care Needs Benefit” message is different from the “Handicap” attribute.
Back to top